Postpartum Depression
- Trista Johnson
- May 4, 2020
- 10 min read
Updated: Jul 23, 2021
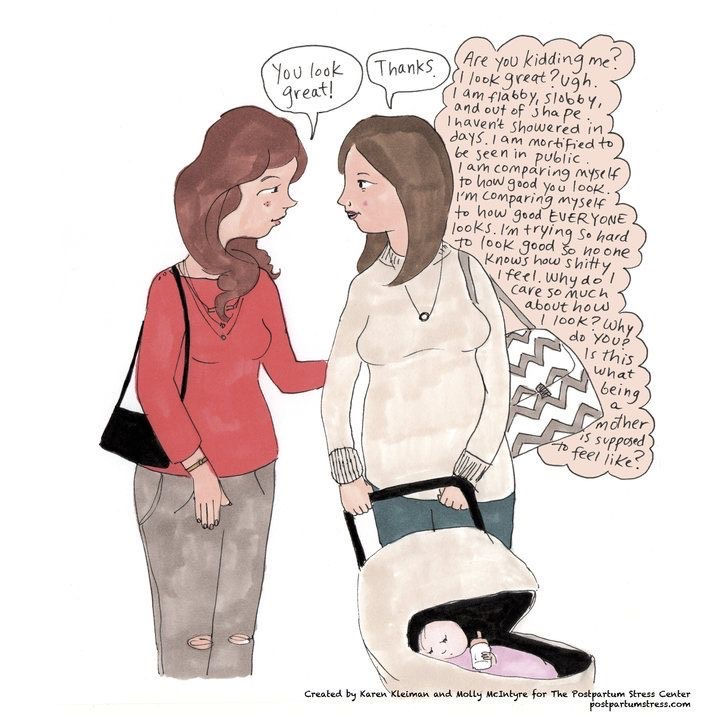
Some people hear the phrase “postpartum depression” and it makes them cringe. It’s taboo. It’s as if there’s this expectation that, because you just had a baby, then life should be nothing but sunshine and rainbows.
Well I’m here to tell you it’s not.
The postpartum period can get really dark, really fast. You just spent the past nine months carrying this tiny little life force inside of you, only to find yourself a stranger to your own body at the end of it all.
Don’t get me wrong, giving birth to my daughter was the most beautiful and amazing experience I’ve ever had. Knowing I was seconds away from finally seeing my baby face-to-face was exciting, but the second she was here and the nurses stripped her from my arms, I was left feeling nothing but empty.

No more little kicks. No more flutters. My stomach had deflated and I was left alone in a dark room as my baby was wheeled away to the NICU.
No more beeping monitors. No more sound of her heartbeat beating rhythmically through the NST machine. Nothing more than one bright light shining down on me, bloodied towels left kicked to the corner of the room and the silent hum of the TV above me.
I remember looking down at my arms, the place where I had held my child for all of five seconds before the nurses pulled her away to place an oxygen mask over her face and move her onto a separate infantile hospital bed. There had been a crowd of nurses moving around her and the only glimpse I had of my daughter was between their moving bodies, catching sight of the oxygen mask and bulb suction being passed between hands.
We didn’t get to have any skin-to-skin contact - a moment that I had been craving for weeks.
Would that prevent my baby from knowing who I was? Would our connection be broken?
I sat alone in that dark room for what felt like forever. The head nurse came in every once in a while to check in on me, but I don’t remember much of what she said. She had simply become background noise at that point. I just wanted to know where my baby was.
The standard length of hospitalization for a woman who has just given birth is 24 - 48 hours (or up to 4 days if you had a cesarean section).
I made it out in 15 hours flat.
The doctors thought I was crazy. My case manager was worried about my mental health. But I didn’t care. The first time I got to hold my baby was hours after she had been rushed into the NICU. I walked into the pod only to find my tiny little 5 pound baby tangled up between a dozen chords, an IV sticking out from her petite little hand and a tube protruding from her mouth, pumping a greenish-brown fluid into a jar.
She was beautiful. But I could also see she was very, very exhausted. I wasn’t allowed to feed her just yet since the doctors wanted to monitor her bowels before clearing her. Again, I began to worry about whether or not my baby and I would be connected since there were so many barriers being placed between us.
It felt like I was given very little time to spend with my newborn baby, as the doctors had decided it was time to transport her to the children’s hospital out of fear of her having a bowel obstruction. Before I had time to process anything, a bed had been reserved and a call was placed for the air-vac team to come pick up my daughter and carry her away from me.
I felt like I was bound and shackled to the hospital as the paramedics rolled in the “carriage” and strapped my daughter in. She would be carried off to another hospital while I would be stuck in one place.
Feelings of emptiness and loneliness continued to loom over my head.
I think the doctors saw me break down in my husband’s arms while the paramedics prepped my daughter for transport. One of the medics handed me a blanket as a keepsake, but nothing would make me feel better in knowing I wasn’t going to get to spend those first precious hours with my baby. I think they all took pity on me and that’s the only reason why they discharged me early.
I rushed through clipboard after clipboard’s worth of paperwork as nurses droned on in the background about being discharged so soon, warning signs to look out for and not being able to be sent home with any pain medications given I was technically leaving against medical advice.
I didn’t care. I just wanted to get out.
I remember they screened me three different times for postpartum depression, but I never took note of the fact that my answers were slowly moving further and further down the scale into the danger zone. I couldn’t allow myself to think or feel anything when my daughter needed to be my main focus. She was the one experiencing trauma, not me.
My daughter spent eight days in the NICU at the children’s hospital. Those eight days were the hardest mentally, emotionally and physically. It hurt to walk. I felt pains in random places of my body. Why are my armpits sore? This makes no sense. Using the bathroom was a joke. Remember that postpartum commercial that was banned from being aired during the Golden Globes? Maybe it’s TMI, but they totally should have aired that bad boy because postpartum bathroom breaks are an absolute nightmare.
Each time, I was reminded that my body was never going to be the same. I remember looking in the mirror my first night home. My stomach was the equivalent of being four months pregnant. I could see my toes again, but that also meant I could bend over far enough to see stretch marks had erupted in places they didn’t originally exist before. That dark line falling down the center of my stomach was daunting.
It’s difficult to admit - but this body that gave life was also one I didn’t recognize anymore. I felt like a stranger, but, most importantly, I felt empty.
I laid in bed those first few nights postpartum with my hands on my belly waiting for the little kicks that would never come. I carried my baby for 38 weeks, and now she was alone in a NICU bed while I was laid comfortably in my own. I felt guilty knowing the only company my daughter would have during the evening hours was the team of nurses ushering in and out of her room. My husband and I would spend the entire day by her bedside, but once it came time to leave, I couldn’t help but feel like I was abandoning her.
“You guys are going to be grateful for the silent nights soon enough! Just wait!”
That’s what people used to say when I talked about going home at night without my baby. Yes, the house was quiet. But I hated it. I know waking up to feed and pump every 2-3 hours is rough, but I’d rather be exhausted than be without my baby. The silence is exactly what was keeping me up at night.
It certainly didn’t help being holed up in a dark and windowless room each day. It was easy to lose track of what time, or even what day, it was. Everything just blended together and it felt like we were living in an endless loop of darkness. I could feel the exhaustion creeping in, but I chalked it up to being normal for a parent of a NICU baby. I didn’t think I needed help. I felt embarrassed even asking for it.
I needed to be tough.
The day the doctors finally approved my daughter for discharge was the longest day of our NICU stay. It felt like all odds were against us. The nurses had no clue what they were doing. Her insurance wasn’t approving her medications. Case managers weren’t pulled into the loop until the night shift was ready to move in. Everything was hectic and unorganized, and I was getting ready to snap. The pod was beginning to feel suffocating and I just wanted to get out.
I thought I would feel relief once we made it home with our bundle in tow, but it seemed like my anxiety only got worse from there. I was happy to finally be free of all the alarms, machines, chords and IV’s, but then there was also a part of me who worried my daughter’s vitals would drop and we wouldn’t know without the beeping of any monitors. I found myself placing my hand over her sleeping body every ten minutes to make sure she was still breathing. I couldn’t stop looking at her. I didn’t want to. I felt the need to make up for the time lost between both hospital stays, while also worrying constantly that, somewhere, a bomb would detonate and we’d end up right back in the hospital.

Every little noise had my leaping up from bed and rushing to her bassinet to pull her out and make sure she was okay. Every sneeze, grunt and coo would startle me out of whatever I was doing and send me straight into a panic.
“This is normal,” I told myself. It was normal for a new mom to worry this much. I didn’t need to tell anyone. I didn’t need to ask for help. I’d be silly to do so.
This is normal.
But, oh, how wrong I was! This certainly was not normal. In fact, my fear and anxiety was pushing me further and further away from both my husband and child. Thoughts of wanting to hole up and disappear flooded my head, placing me in a state of mind that was so unfriendly and distant.
People would ask me how I was doing. I would lie and say I was okay. I chalked everything up to being tired.
Tired was a normal emotion for new moms, right?
I found myself holding back tears constantly, whether it was because of something I saw on TV or something as minuscule and dropping my baby’s pacifier on the floor. I felt overwhelmed with negative emotions and I didn’t know where they were all coming from. At one point, I found myself standing in our kitchen pantry, sobbing heavily, while my husband sat there and held me.
I still don’t know what set me off.
For weeks, I felt like I was silly for feeling so emotionally unstable. I had a baby who needed her mother to be strong. I felt like I was selfish for being this way and it only made it harder for me to want to talk to anyone.
When I went to my OB for a four week follow up, they screened me again for postpartum depression. Reading through the questionnaire for what felt like the millionth time, I noticed that my answers had shifted. I thought about changing them at the last minute before the doctor came in, but decided not to. Maybe it was time to get help...
The doctor walked in, took one look at me before burying her face into her laptop and proceeded to ask me a series of generic questions about my labor and delivery experience.

“When was the baby born?”
“What was the gender?”
“How much did she weigh?”
“Did you need any stitches?”
“How is the bleeding?”
Not once did she ever address the postpartum depression screening I had handed back to her. Instead, the papers sat amongst a bundle of other packets on the corner of her desk.
She never looked at them. She hardly even looked at me.
After that appointment, I went back to thinking my emotions needed to be placed under better control. Why was I even considering the idea that I might be depressed? This wasn’t about me. There were bigger fish to fry.
I needed to put my big girl pants on and move on.
Another week passed. I ate less. Tended to myself less and less. I became a robot.
Wake up. Feed the baby. Watch her sleep. Repeat.
The reality of my situation didn’t hit until I received a video call from one of the nurses on our high risk postpartum team. She asked me how I was feeling and, without warning, the flood gates opened. I found myself crying without being able to stop. I apologized to the nurse and told her I was simply feeling overwhelmed with my daughter’s medical management plans and worrying about something bad happening to her. I opened up about the nightmares I was having about dropping babies or losing them in a crowd of people. I told her I felt like I was panicking all hours of the day. I told her I was concerned my connection with my daughter had been hindered by the skin-to-skin contact that was denied to me at birth.
I told her I knew it was just normal first-time-mom emotions.
She told me I was wrong.
“These are all signs of postpartum depression,” she advised me. She urged me to quit apologizing for having cried and emotionally unloading on her. “This is what our team is built for. Now let me help you.”
She continued to remind me that this was nothing to be embarrassed about. Sure, there’s a stigma around postpartum depression and no one really likes to talk about it - but it was also important that I got back to feeling like myself again so I could enjoy these precious milestones with my baby. Lord knows they’re only little for so long.
She advised me to open up to my loved ones about how I was feeling and what I was thinking. Knowing I was pursuing a degree in English, the nurse also urged me to begin keeping a journal of my thoughts.
“Even if no one reads it, it’s important to recognize that your feelings are real and deserve validation, even if that validation only comes from you.”
It seems silly now that I look back on the past seven weeks. There’s really no point in hiding the fact that my mental and emotion health was hindered by my pregnancy, labor and delivery experience. My daughter was diagnosed with a rare genetic condition and we have spent the first weeks of her life being consumed by doctors, lab tests, monitors, IV’s, and medical imaging.
There’s a lot of trauma there and I shouldn’t have to feel weak for admitting that. I know no one would have ever denounced what I was feeling. Everyone would have been supportive. The only real enemy here was myself and the stigma I was letting dictate what I opened up about and to whom.
I was so dead-set in putting on a brave face that I was slowly breaking myself down.
And that’s not okay.
This week, my nurse was happy to hear that I had finally chosen to write about my experience in both having a NICU baby and how it impacted my postpartum depression. She was even more excited to hear about my decision to share it publicly.
“We need more advocates in this field,” she said. “We need more people to talk about postpartum depression so it’s not such a taboo subject anymore. This is not something we should feel awkward discussing when talking about it could save someone’s life.”
For assistance with handling postpartum depression, call the Postpartum Warm Line at 1-888-434-MOMS (6667).
Dads are welcome to call too.
Mental health matters, no matter the circumstances.






Comments